|
If the current warnings about upcoming meat shortages make you uneasy, you aren’t the only one. Many of us, especially those with irritable bowel syndrome (IBS), don’t digest the most common source of plant-based protein (beans and lentils) very well. Having no access to meat can conjure up images of bloated bellies, painful abdomens, and flatulence… And who wants more of that? Luckily, many of us CAN transition to eating more legumes (including beans, lentils, and peas) with few side effects, if we do so in a controlled and intelligent manner. I know it’s possible because I myself could not digest them very easily only a few months ago and have made some progress in the last couple of months! Why Legumes Are Difficult To Digest There are various reasons why legumes are more difficult to digest.
Your Gut Microbiome Changes With Your Diet The makeup of your gut microbiome (that fine balance of microbes that create a diverse “garden” in your digestive system) changes based on what you are eating. If you aren’t used to eating beans, then you won’t have many bacteria in your gut that will help you digest them. Makes sense, no? So, if possible, it would be less painful to slowly add more plant-based protein into your diet rather than changing everything overnight. This gradual process will allow your gut microbiome to slowly adjust and grow the type of bacteria that will be helpful to you as you embark on this change in your diet, with minimized bloat. Try once a week, then twice a week, moving forward if you seem to be doing well. The changes in your gut bacteria can start to occur within one week of starting to eat more legumes, but will revert if you stop. Which Legumes Are Best To Start With? The ”sweeter” legumes, those that are typically associated with sprouting, are usually considered more digestible. Lentils have been my first go-to. Others in this category include adzuki beans, mung beans, and black-eyed peas. Those that tend to be most difficult to digest have a harder outer skin, and include lima beans, soybeans, and navy beans – leave these to when you are a pro! Cooking Hacks To Make Your Legumes More Digestible If you’re ready to give legumes a shot, here are a few tricks to make them more digestible:
Hopefully this was helpful to you! And don’t forget about other sources of vegetarian protein, including hemp hearts, other nuts and seeds, and eggs that you can rely on while you work on the legumes. If legumes are your nemesis, you may benefit from specific digestive enzymes and digestive support. You may also be dealing with a more complex issue such as irritable bowel syndrome (IBS) – just get in touch and I can help! In health, Dr. Tamar References Holscher H. D. (2017). Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut microbes, 8(2), 172–184. https://doi.org/10.1080/19490976.2017.1290756 Messina, V. (2014). Nutritional and health benefits of dried beans. Am J Clin Nutr, Jul, 100 Suppl 1, 437S-442S. . doi: 10.3945/ajcn.113.071472 Samsel, A., & Seneff, S. (2013). Glyphosate, pathways to modern diseases II: Celiac sprue and gluten intolerance. Interdisciplinary toxicology, 6(4), 159–184. https://doi.org/10.2478/intox-2013-0026 Tomova, A., Bukovsky, I., Rembert, E., Yonas, W., Alwarith, J., Barnard, N. D., & Kahleova, H. (2019). The Effects of Vegetarian and Vegan Diets on Gut Microbiota. Frontiers in nutrition, 6, 47. https://doi.org/10.3389/fnut.2019.00047
0 Comments
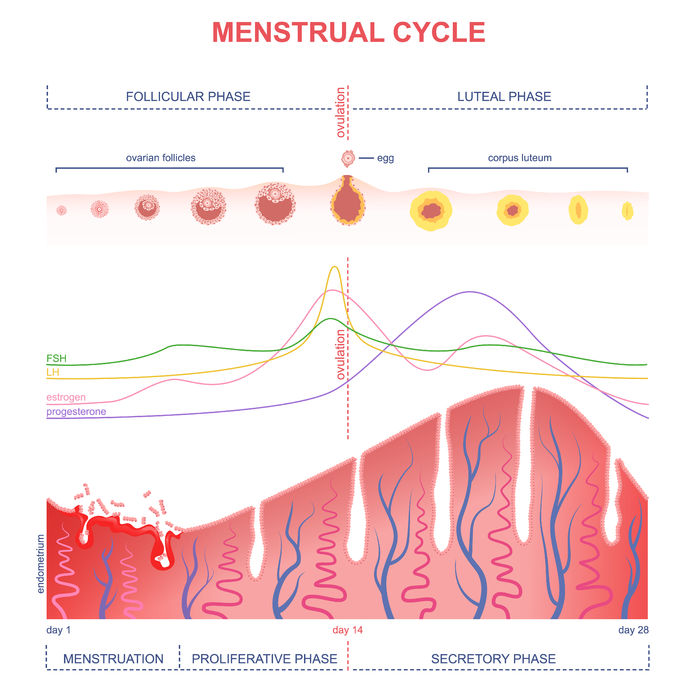
It’s something many women have resigned themselves to tolerate and live with, or at least until periods do us part. The heavy periods, the “flooding”, the fatigue associated with it, and sometimes the monthly requirement for sick days. Many women don’t know what’s normal and are not given any many options to deal with them other than anti-inflammatories, the birth control pill, endometrial ablasion, or a hysterectomy. However, naturopathic medicine opens up a myriad of treatment options, which need to be targeted to you and the reason why you are getting heavy periods in the first place. I am a big fan of testing in the right context, since it allows us to then create a more targeted and more effective treatment plan for you. Women can start getting heavy periods at different points in their reproductive lives, but what I will be covering today is the tendency towards heavier cycles which tends to occur as women start the transition towards menopause. If you’re nowhere near your 50’s, this could still apply to you: perimenopause can start up to 15 years before your periods actually stop! So, many women in their late 30’s start to experience symptoms. Menstruation 101 Most women have only a very basic understanding of what goes on in their bodies during every menstrual cycle. So that you can breeze through the rest of this blog, let’s give you a rundown of the basics first, shall we? (Psst… Skip over this section if you’re all in the know!) To begin, by convention, the first day of your menstrual cycle is the first day of your menstrual flow. If you have a day or two of spotting before your full flow starts, those spotting days are part of the previous cycle.
The two main key players produced in your ovaries are estrogen and progesterone. Estrogen is the predominant hormone in the first half of your cycle until you ovulate, and then progesterone rises and becomes the predominant hormone (along with a second rise in estrogen). Your uterine lining, which prepares for the possibility of a pregnancy every month, goes from being very thin right after menstruation, to thickening up, maintaining after ovulation, and then shedding at menstruation. If you think of the lining of your uterus as a lawn, think of estrogen as the fertilizer which helps your uterine lining grow, and progesterone as the lawnmower which keeps the growth in check. Estrogen = fertilizer Progesterone = lawnmower What happens in perimenopause? The problem is that in perimenopause, progesterone levels start to dip, usually before estrogen starts to dip significantly. This progesterone dip has to do with irregular ovulation or the poor quality of the eggs that are released. Chronic stress can also decrease your progesterone production. Fertilizer + no or little lawnmower = out of control lawn = heavy periods What is an unusually heavy period? Before we delve into testing, let’s clear up one thing: what defines heavy periods, or “menorrhagia”? -Losing more than 80mL of blood during your period -Soaking a pad or tampon every 2hrs or less And/or -Your period lasts more than 7 days Test, don’t guess If you find yourself in this situation, here are some of the top 3 tests that I would likely order to shed light into what is causing or contributing to your heavy periods.
There are other causes of heavy periods, like clotting disorders, fibroids, polyps, or uterine cancer which can be more fully evaluated through a medical doctor due to their access to testing or imaging. If any of these are suspected, then I would refer you to your medical doctor. Once we know what is going on, we can use our naturopathic tools to help lighten your period and make this transition in your life as manageable as possible! Herbs, nutritional supplements, dietary changes, bio-identical progesterone, and acupuncture can all be helpful to manage heavy perimenopausal periods. If you’re currently navigating this perimenopausal period of your life and are looking for natural solutions, give us a call and I will be delighted to help you. References: Image from 123rf.com Livdans-Forret AB, Harvey PJ, Larkin-Thier SM. Menorrhagia: a synopsis of management focusing on herbal and nutritional supplements, and chiropractic. J Can Chiropr Assoc. 2007 Dec;51(4):235-46. “Doc, I think I have a hormone imbalance.” The majority of the women I see in my practice first come in with some form of hormone-related concern. If they are in their reproductive years, they may suffer from PMS, spotting between periods, painful periods, PCOS, cyclical acne, or irregular periods. In their pre-menopausal years, their period may still come but irregularly, accompanied with hot flashes, insomnia, lowered thyroid function, and other symptoms. Once in menopause, women still experience symptoms related to changes in their hormones. Resolving those imbalances can seem complex and overwhelming at times, but never underestimate the power of what you put at the end of your fork: your food. One of the first dietary tools that I recommend to patients to help balance hormones is called seed cycling. I have seen this alone have a positive impact within 3 months in patients who do just that! Of course, most cases are much more complex and necessitate a multi-pronged approach. But the effectiveness of this simple and low cost therapy as a starting point should not be overlooked. What is Seed Cycling? Seed cycling uses specific estrogen-balancing and progesterone-balancing seeds at different times of your menstrual cycle in order to help shift and improve hormone imbalances. It is as simple as incorporating a total of 2 Tbsp of the specific seed(s) (I usually recommend a raw form) once a day, switching seeds halfway through your cycle, around ovulation. Why do we switch seeds? The beginning of your menstrual cycle is the first day of your period (Day 1). From Day 1 until ovulation (typically around Day 14 IF you have a textbook 28 day cycle), the predominant hormone is estrogen, which helps build up the lining of your uterus (the endometrium) after your period. Flaxseeds and/or pumpkin seeds help to balance estrogen levels and are therefore used in this first half of the cycle. From ovulation until your period starts is the second half of your cycle, in which progesterone is more predominant. This is why we switch to the progesterone-balancing seeds, sesame and/or sunflower seeds. A typical cycle will look like this:
-Day 1-14 (follicular phase): 2 Tbsp (total) of freshly ground flaxseed (or whole pumpkin seeds) – estrogen balancing -Day 15-28 (luteal phase): 2 Tbsp (total) of sesame or sunflower seeds – progesterone balancing You can use a combination of the seeds (1Tbsp of each), or just stick to 2Tbsp of one kind in each category. If your cycle is not 28 days, and/or you have no clue when you ovulate, then you will need to start charting your cycle (using markers such as cervical mucous +/- basal body temperature), in order to find out your particular pattern and whether it falls within the normal range. I like the Kindara App to help with tracking this, but there are many other apps out there, or you can you good old pen and paper charts too! How Does It Work? You might be asking yourself if taking these little seeds daily can really have an impact on your hormones. After all, if you go to your medical doctor to try and “balance hormones”, you will usually be recommended some form of birth control. This actually does not balance your hormones at all, but it suppresses your natural production of hormones in order to try and prevent the process of ovulation, fertilization, and make the uterus lining inhospitable to embryo implantation. Furthermore, the birth control pill sets you up for specific vitamin and nutrient deficiencies, as well as imbalances in your gut flora (the good bugs that help regulate your immune system). Therefore, if your goal is to balance hormones, the birth control pill is not your answer. Although there are no studies of the seed protocol itself, we do know from studies of the individual seeds how they may be gently nudging our hormones in the right direction. -> Flaxseeds Most women tend to have estrogen dominance, too much of the hormone estradiol, which can manifest as fibroids, endometriosis, mood swings, hair loss, breast tenderness during PMS, and even an increased risk of estrogen-positive cancers such as breast and ovarian cancer. Flaxseeds are considered a “phytoestrogen”, but they don’t directly boost all estrogens as the name might lead you to think. They actually decrease the production of the more harmful estrogen form of estradiol, as well as shift the balance of estrogen metabolites (breakdown materials) from the more harmful 16-hydroxy-estrone towards the less harmful 2-hydroxy-estrone. What they are actually “boosting” is the more beneficial estrogen metabolites… Win-win! Ground flaxseeds have been shown to be helpful for premenstrual breast tenderness and to decrease estrogen-dependent cancer risk. -> Pumpkin and Sesame Seeds Similarly to flaxseeds, pumpkin seeds also have phytoestrogens which have shown potential in decreasing estrogen-dependent cancer risk, but they have not been studied as extensively as flaxseeds. Zinc is high in both pumpkin and sesame seeds, and indirectly helps increase your production of progesterone. The corpus luteum (the “shell” that is left over in your ovaries from the egg that is released during ovulation) becomes the main producer of progesterone in the second half of your cycle, but only if you ovulate. Zinc increases progesterone production by stimulating the hormone FSH, which is needed for proper ovulation to occur. -> Sunflower Seeds Sunflower seeds are high in selenium, magnesium, Vitamin B6, Vitamin E, and also contain a decent amount of zinc. These nutrients are needed for proper progesterone production and hormone metabolism. How To Get Started If you are dealing with some female hormone imbalances and would like to get started with this dietary intervention, you can start at any time! Just make sure to find out what phase of your cycle, follicular (1st half) or luteal (2nd half) phase, you are in, and start consuming the seeds for that phase until it’s time to switch. As these seeds are high in fibre, make sure to have them with plenty of water so that you don’t get constipated. As well, some people experience bloating when they start eating these amounts of ground flaxseeds – if this is you, cut back and start small, working your way up, or try pumpkin seeds instead. If your case is more complicated or you have irregular cycles, it might be worth it to get a proper evaluation. You may need an in-depth hormone assessment through bloodwork, salivary hormone testing, or dried urine testing (DUTCH test) to really find out what is going on. Naturopathic doctors have many tools to help you balance your hormones, including dietary and lifestyle changes, botanical medicines, nutritional supplementation, and acupuncture. As always, I would love to help you get to the bottom of your hormone troubles so that you don’t have to fear that time of the month anymore. Make an appointment at my Brampton office to get started. In health, Dr. Tamar References Haggans CJ, Travelli EJ, Thomas W, Martini MC, Slavin JL. The effect of flaxseed and wheat bran consumption on urinary estrogen metabolites in premenopausal women. Cancer Epidemiol Biomarkers Prev. 2000 Jul;9(7):719-25. Images from 123rf.com. Maleki-Saghooni N, Karimi FZ, Behboodi Moghadam Z, Mirzaii Najmabadi K. The effectiveness and safety of Iranian herbal medicines for treatment of premenstrual syndrome: A systematic review. Avicenna J Phytomed. 2018 Mar-Apr;8(2):96-113. Mojgan Mirghafourvand, Sakineh Mohammad-Alizadeh-Charandabi, Parivash Ahmadpour, Yousef Javadzadeh. Effects of Vitex agnus and Flaxseed on cyclic mastalgia: A randomized controlled trial. Complementary Therapies in Medicine; Volume 24, 2016: 90-95. Richter D, Abarzua S, Chrobak M, Vrekoussis T, Weissenbacher T, Kuhn C, Schulze S, Kupka MS, Friese K, Briese V, Piechulla B, Makrigiannakis A, Jeschke U, Dian D. Effects of phytoestrogen extracts isolated from pumpkin seeds on estradiol production and ER/PR expression in breast cancer and trophoblast tumor cells. Nutr Cancer. 2013;65(5):739-45. Sicilia T, Niemeyer HB, Honig DM, Metzler M. Identification and stereochemical characterization of lignans in flaxseed and pumpkin seeds. J Agric Food Chem. 2003 Feb 26;51(5):1181-8. Wzelaki, Magdalena. Seed Cycling to Balance Pre and Post Menopausal Hormones. Dr. Jolene Brighten. 2009-2019. Accessed Jan 22, 2019: https://drbrighten.com/seed-cycling-menopausal-hormones/. As we head into the thick of winter, spending our time indoors and less time in the sunshine, we can be more prone to those pesky cold and flu viruses. Nobody likes feeling run down with runny noses, congestion, cough, fever, or body aches. What if you knew of a low-cost treatment that could help boost your immune system while you sleep? Read on so that you’re in the know! This “warming sock” treatment is an old hydrotherapy technique that helps increase circulation, decrease nasal congestion, improve fevers, and improve the effectiveness of your immune system to fight off viruses. Many of those who have tried it also find that they sleep much better! However, you will soon find out that the “warming socks” term is a euphemism… You will actually be putting cold wet socks on your feet, but they won’t stay wet for long as you will end up drying them while you sleep, with the help of dry wool socks and tucking into warm blankets. While the idea of putting cold wet socks on your feet may make you cringe (trust me, I get you on that one!), if you actually follow through, you should feel much better! Just follow the extra tips I give you in my instructions, and you should have smooth sailing. What You Will Need: -1 pair of THIN cotton socks -1 pair of THICK wool socks -Hot water foot bath (or alternate way of warming your feet) -Towel -Warm blankets -A bit of courage Instructions: 1) Get ready for bed. Getting the warming socks on should be the last thing you do before you tuck yourself in. 2) Warm your feet in a hot foot bath for 5 min (or using an alternative method). 3) Dry your feet well with the towel. 4) Run your thin cotton socks under cold running water to get them wet, then wring them out thoroughly. Don’t skip the wringing step – there should be no more water dripping from them! 5) Take the wet cotton socks and dry wool socks to the bedside. Make sure your feet are still warm and toasty. Don’t proceed unless they are! 6) Put on the wet cotton socks. 7) Follow immediately with the dry thick wool socks. 8) Tuck yourself into bed with warm blankets. Make sure not to get chilled. 9) Go to sleep for the night. 10) Do this 3 nights in a row (ideally). What Can You Expect? You should wake up the following morning with dry socks since your body increased circulation towards your feet to keep you warm. This pulls the congestion away from your head, decreasing the nasal congestion symptoms. It also leads to improved immunity (the hot/cold contrast helps improve the effectiveness of your white blood cells to fight bacteria and viruses), and less cold and flu symptoms. The best time to start this is at the first sign of a cold or flu, but you can start anytime. Disclaimer: If you have a chronic health condition or another serious medical condition, make sure to check with your doctor before starting this treatment. If you try this treatment and your symptoms get worse, also be sure to check with your doctor. This is just one tool that naturopathic doctors have to help you get over colds and flus fast. If you want an individualized plan of action to help you get over colds and flus fast this winter, make sure to book in and we will put together a strategy plan for you! In health, Dr. Tamar Reference: -Image from 123rf.com You hear that familiar wheeze or cough although you barely did any exercise. You may have just gone up a set of stairs, stepped out into the cold, or emptied out the dust compartment of the vacuum cleaner. Here it goes again, you think, as you reach for your inhaler…
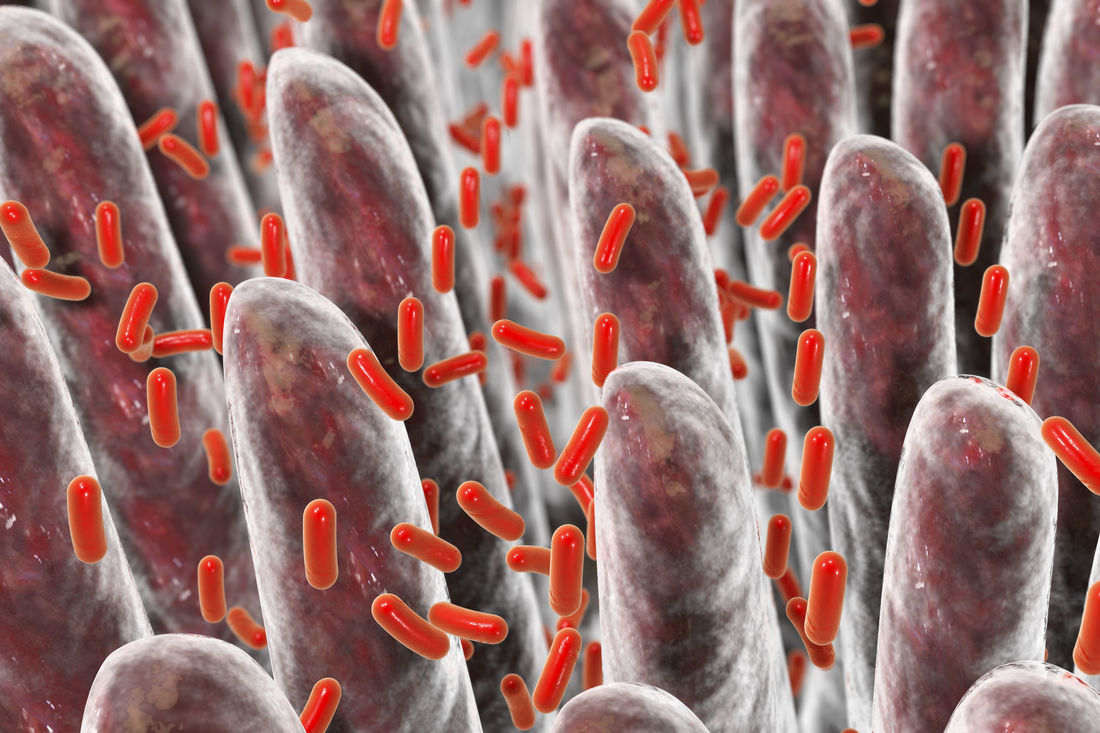
Your thyroid is a master gland at the base of your neck which helps control your metabolism. If your thyroid function is sub-optimal (on the low side), you may experience symptoms such as fatigue, difficulty losing weight, depression, foggy thinking, hair loss, cold extremities, and feeling burned out. This could be the case even if your thyroid tests look “normal” by conventional standards.
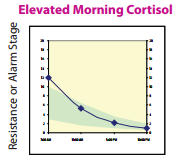
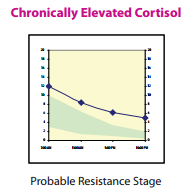
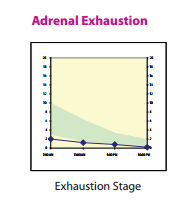
If your thyroid hormones are truly out of the “normal ranges”, you will most likely be prescribed Synthroid or levothyroxine, which is a synthetic form of the thyroid hormone, T4. However, this T4 needs to be converted into the active thyroid hormone, free T3. Many patients that I see have T4 levels that look fine or even on the high side of normal, but they still have symptoms. Giving them more T4 won’t help! We need to promote the proper conversion of T4 into T3, and some patients do better when we switch them from Synthroid to Desiccated Thyroid (which contains a little active T3 in it). So, here are 5 ways to help improve that T4 to T3 conversion, in order to boost your metabolism! 1) Get enough sleep If you aren’t getting enough sleep, you aren’t giving your body a chance to produce enough Growth Hormone (produced in your slumber). Growth Hormone increases that T4 to T3 conversion. If you’re having trouble sleeping, you could also have a melatonin deficiency, a hormone which you produce when it is dark and which helps make you sleepy. Melatonin is also needed for proper T4 to T3 conversion. 2) Get adequate protein in your diet Protein is essential as a building block for tissue repair and proper enzyme function in your body. The average person needs about 60-70 grams of protein per day. You can get this from lean protein sources such as fish, chicken, eggs, nuts, hemp hearts and other seeds, and legumes (however, if you have an autoimmune thyroid issue, some of these may not be recommended). Avoid soy protein sources, especially the non-fermented ones, as they can slow down thyroid function. Enough protein in the diet helps build muscle, decreases fat storage, improves satiety, decreases cravings for sweets, and helps burn more calories. 3) Balance your blood sugar Foods high in sugar or refined carbohydrates (found in processed foods, white flour, fluffy breads, bagels, and most baked goods) spike up your blood sugar, which leads to insulin being released to help bring the sugar into your cells. Guess what insulin does… It decreases the conversion of T4 into T3, resulting in less active thyroid hormone! Eating a mostly plant-based, unprocessed diet, with adequate amounts of protein, helps to balance blood sugar levels, keeping them more steady and avoiding the big insulin-triggering spikes. 4) Decrease stress Chronic stress leads to the production of the stress hormone cortisol. Cortisol interferes with proper metabolism in several different ways. First of all, it decreases the conversion of T4 into T3. It also shunts some of the T4 away from producing T3, and into producing reverse T3 instead. Reverse T3 functions as a brake on metabolism! Also, chronic stress decreases the ability of insulin to effectively bring sugar into the cells, leading to more insulin being needed for the same effect (insulin resistance)! 5) Optimize essential nutrients and vitamins (especially selenium, iodine, zinc, iron, Vitamin A, Vitamin B12, Vitamin D) These essential nutrients are very important for producing enough thyroid hormone, and some are also useful if there is an autoimmune thyroid issue such as Hashimoto’s thyroiditis. Work with a naturopathic doctor to ensure you have optimal levels of these, supplementing when necessary. It is possible to take too much of these too, so make sure you’re taking the right amounts for you! Still feeling sluggish and having trouble losing weight? I can help! Working with a naturopathic doctor can help you eliminate the guesswork, get some testing done, and approach your goal in an individualized and systematic way. There are so many factors as play regarding metabolism, many of which I did not mention here. Come on in for a visit, and we’ll get you started on a program tailored for you! References Bray GA, Smith SR, de Jonge L, Xie H, Rood J, Martin CK, Most M, Brock C, Mancuso S, Redman LM. Effect of dietary protein content on weight gain, energy expenditure, and body composition during overeating: a randomized controlled trial. JAMA. 2012 Jan 4;307(1):47-55. Image from 123RF.com, Copyright: <a href='https://www.123rf.com/profile_magone'>magone / 123RF Stock Photo</a> Scott, TD, Speidel, K. (2017). Essential Elements of Prescription Hormone Compounding. LP3 Network. Conference 2017 Apr 29-30. We have all heard about probiotics, and how good they are for us. We have probiotic yoghurts, fermented foods, kefir, and probiotic gum easily available to us. After taking antibiotics, many of us know that it’s a good idea to replenish our good bacteria and load up on probiotics. As a naturopathic doctor, a recommendation for a good quality daily probiotic is very common for most of my patients. However, there is a subpopulation of my patients for which this is NOT a good idea. At least, not initially. These patients actually have an overgrowth of bacteria in the small intestine, and giving them probiotics can actually make them worse if we don’t treat the underlying condition first. Most of these patients have already been diagnosed with Irritable Bowel Syndrome (IBS). However, the diagnosis of IBS doesn’t actually tell them what is causing it, just that their bowel is irritable and that they most likely don’t have a more serious condition. Since I have started testing for it, I have found that many of my IBS patients actually have Small Intestinal Bacterial Overgrowth (SIBO) as the underlying condition. Furthermore, even if you have a diagnosis of Celiac disease, Colitis, or Crohn's, you may still have SIBO: those with these conditions actually have a 3-fold increased risk of developing SIBO, because of all of the gut inflammation, and its effect on the nervous system surrounding the digestive tract. So, what might be some indications that you might have SIBO? 5 Key Clues That May Indicate SIBO 1) Bloated all the time You may start off the day with a relatively flat stomach, but as the day progresses, you go up a few sizes and may look pregnant! This might happen no matter what you eat. Or, you may have identified a few foods that make things worse, but even when you avoid them, you still get some digestive symptoms. 2) You feel worse with high fibre and/or sugary foods A diet high in fibre can lead to increased fermentation of food by bacteria in the small and large intestines, and if you already have an overgrowth of bacteria, you can imagine that this could lead to increased gas. Sugary foods, and/or foods high in certain types of carbohydrates (high FODMAPs foods), also feed the bacterial overgrowth, and can worsen symptoms. And it’s not just bloating that you could experience. Depending on the predominant type of bacteria present, hydrogen-producing of methane producting, you could also experience diarrhea and/or constipation, or even heartburn. 3) You have a history of bacterial gastroenteritis If you’ve had a bad stomach bug, or haven’t been well after “traveller’s diarrhea”, this may have set off the fine balance in your gut and contribute to SIBO. You may have also been put on strong antibiotics, which can kill off some of your good bacteria and allowed less beneficial bacteria to thrive. 4) Your thyroid is sluggish You may have been diagnosed with hypothyroidism, or have sub-laboratory hypothyroidism (your thyroid function may not be slow enough to be prescribed Synthroid for it, but you have symptoms). Either of these can slow down your digestive system and the transit time down the digestive tract, allowing bacteria more time to ferment it. 5) Taking probiotics makes you worse This makes sense, as, if you have an overgrowth of bacteria in the small intestine, populating with more bacteria, even the “beneficial” ones, could make things worse. Not everyone with SIBO gets worse with probiotics, but most SIBO patients don’t feel significantly better on them if we don’t get rid of the overgrowth first and make sure that the sweeping function (migrating motor complex) of the small intestine is working properly beforehand. Does this sound like you? Have you been struggling with ongoing digestive issues but haven’t had a breakthrough yet? Come on in for an assessment, and we’ll see if testing for SIBO would be a good idea for you! References: Image from 123rf.com, Copyright: <a href='https://www.123rf.com/profile_drmicrobe'>drmicrobe / 123RF Stock Photo</a> Khangura, P. (2017). Superseding SIBO. Webinar 2017 May 13. You’re feeling overwhelmed, your body doesn’t listen to you anymore, you’re exhausted but you can’t sleep, you’re gaining weight around the belly, and you have your suspicions that chronic stress is to blame. You may have read my previous blog about adrenal fatigue, and figured that your adrenal glands are likely getting exhausted from working overtime to help you cope in a stressful world. But the symptoms of adrenal fatigue are wide and varied. How can you test and find out how healthy your adrenal glands really are? Furthermore, how do you find out which stage of adrenal fatigue you may be in? Hormonal Questionnaire I use a ranked questionnaire shared by Dr. Tara Scott and Dr. Ken Spiedel at a conference I recently attended, which uses symptom severity and an algorithm to figure out your most predominant hormone imbalances. While this is not a fool-proof test, it allows us to get an idea of what are most likely to be your top 3 hormone imbalances. The results from this simple questionnaire tend to correlate well with the results from hormone testing, helping direct further objective testing. It can help us identify if most of your symptoms are likely from too high cortisol, too low cortisol, both, or something else altogether. In-Office Testing During a physical exam, there are a few specific tests I can do that indicate if you are likely in Stage 3 adrenal fatigue, where your cortisol production goes down. The first test looks at your pupil’s reaction to light. I shine a light in your eye, and see if you can maintain your pupil’s constriction for a short period of time. If you can’t, or your pupil closes and then opens in this time frame, this is one possible indication that your adrenal glands are fatigued, as it correlates with your adrenaline levels (also produced by the adrenal glands). The second test I do in-office is checking your blood pressure lying down, and then standing up (called orthostatic blood pressure). Generally, when you get up, you should be able to bring your blood pressure up by about 10 points within one minute. If it stays the same or goes down, it could be a sign of hypoadrenia. Again, other factors can affect this, including medications that you’re on. This test will likely be positive (blood pressure will stay the same or go down when you get up) if you are in Stage 3 adrenal fatigue. However, if you’re in Stage 1 or Stage 2, or even early Stage 3 adrenal fatigue, this test may still look normal. Salivary Hormone Testing Salivary hormone testing for cortisol and its precursor, DHEA, is the preferred method for testing adrenal function. Cortisol is the main hormone produced by the adrenal glands during chronic stress. There are several advantages of this method over doing a blood test for cortisol: 1) Salivary testing avoids falsely elevating cortisol levels from doing a blood draw. Pricking or lancing has been shown to increase cortisol levels just because of the anxiety the procedure causes for many people, whereas spitting into a tube in the comfort of your own home usually does not. 2) Salivary testing can be done several times throughout the day, allowing us to see the normal (or abnormal) daily variation of cortisol. Blood is not convenient to test more than once during the day. However, cortisol levels usually are highest in the morning, and then decrease during the rest of the day. Seeing where your levels fall at 4 different time points allows us to more accurately assess which stage of adrenal hypo-functioning you may be in.
3) Salivary testing allows us to identify the level of cortisol that is actually getting to your tissues, where it acts (the active cortisol). Blood levels usually use very large “normal” ranges, and include both bound (inactive) and free (active) cortisol. Blood Levels of Cortisol As mentioned above, this is not the preferred method. But, if we want to screen out more serious conditions of the adrenal glands, such as Addison’s Disease (extremely low adrenal function) or Cushing’s Syndrome (abnormally high cortisol), blood tests could be used. Ready To Test? If you suspect your adrenals are near or at burnout, or you are under chronic stress, don’t delay in pursuing treatment with a naturopathic doctor. The health of the adrenal glands is intertwined with that of so many hormones, so make sure you take care of these little soldiers before they’re too exhausted to take care of you! In health, Dr. Tamar References Image from 123rf.com, copyright: <a href='https://www.123rf.com/profile_pixelsaway'>pixelsaway / 123RF Stock Photo</a> Rocky Mountain Analytical (2014). Adrenal Function Panel: Clinical Information for Professionals. January 2014. Scott, TD, Speidel, K. (2017). Essential Elements of Prescription Hormone Compounding. LP3 Network. Conference 2017 Apr 29-30. We all deal with stress. Stressors such as losses, job interviews, presentations, medical diagnoses, lack of sleep, job and home life balance, or challenging relationships can make us feel overwhelmed. Our bodies should be able to deal with these stressors, for a short period of time. And that’s the key: for a short period of time. The problem is, most of us are chronically stressed! How Heavy Is The Burden You Carry? You’ve probably heard of the analogy of holding a glass of water. Hold it for a minute, and it feels light. Hold it for an hour, and your arm will start to ache. Hold it for a day, and your arm will be numb and the glass will feel unbearably heavy. We often don’t remember to put the glass down until it’s too late. Until we have seen the repercussions on our body, mediated primarily by our adrenal glands, these little soldiers that sit on top of our kidneys, trying to fight for us. Fight Or Flight Your adrenal glands perceive any form of stress, whether it is a physical, emotional, environmental, biochemical, or spiritual stress, and respond the same way: by trying to produce either adrenaline (short-term) or cortisol (long-term). They are responsible for our fight or flight response: when our body assesses its environment and deems it unsafe, it prepares us for battle, getting our blood pumping, shifting our resources away from digestion and into our muscles and brain so that we can run from danger or fight it head on. But if this goes on for a long period of time, we will get exhausted, as it’s just not sustainable. How Chronic Stress Affected Me When I graduated from naturopathic medicine, and shortly after writing my licensing exams, my adrenal glands were in rough shape. I had pushed myself through medical school, but once the stressor was over, it was difficult for me to peel myself off the couch or do any exercise at all. I had survived on insufficient sleep, caffeine, deadlines, and willpower, but in the process, my digestion was a mess, and I was constantly battling fatigue throughout the day. Any new stressor made me feel overwhelmed. Luckily, as a new naturopathic doctor, I knew that my adrenal glands were in need of some tender loving care. I was probably near burnout. It took me a good year before I felt a lot better, and a few years more before I felt better than I had years before, during my undergraduate and naturopathic medical school studies. You don’t need to be near breaking point before realizing that your adrenal glands need some help, and that stress is affecting your body in various ways. It’s best to catch it in the early stages, when it’s easier to shift back to balance. Adrenal Fatigue Stages You may have heard of the term “adrenal fatigue” (or adrenal insufficiency, hypoadrenia) from naturopathic doctors and integrative medical doctors. This term really refers to an older concept founded on Dr. Hans Selye’s research (a Canadian endocrinologist), called “General Adaptation Syndrome”. If we are under stress for long enough, we move through the different stages of adaptation to chronic stress, from the alarm stage, to the exhaustion stage. At the end of the exhaustion stage is burnout. You don’t want to get to the exhaustion stage if you can prevent it! Stage 1 – Alarm In this initial alarm stage, the body panics a little and tries to mobilize its resources. You might have a temporary decreased resistance to stress as your body starts to produce more cortisol to deal with the chronic stress, and you mobilize your energy sources from fat and muscle. Some people will lose weight in this stage. Stage 2 – Resistance In this stage, the adrenal glands actually grow in size as they try and keep producing more cortisol. But the high cortisol will wreak havoc on the body. Symptoms of high cortisol include: -feeling tired but wired -anxiety and nervousness; heart palpitations -depressed mood; irritability; mood swings -brain fog, confusion; memory problems; decreased concentration -decreased sex drive -fluid retention -hot flashes; night sweats -hypoglycemia -sleep disturbances -thinning skin -weight gain around the middle -more frequent colds and flus Stage 3 – Exhaustion In this stage, the adrenal glands can’t keep up with the production of cortisol and eventually cortisol production goes down. Any added stressor will be more difficult to deal with, as your resilience goes down. While cortisol levels fluctuate throughout the day, your highest levels of cortisol should be in the morning. Morning cortisol levels are also the last ones to drop in hypo-functioning adrenals. Cortisol helps keep us alert. So if you are having trouble peeling yourself out of bed, and you have late afternoon energy crashes, you may be in this stage. At this stage, you may have symptoms of both low and high cortisol all at once. Symptoms of low cortisol include: -apathy -burned out feeling -anxiety -chemical sensitivities -cold body temperature; cold extremities -cravings for sweets and/or salt -decreased stamina -hypoglycemia -fatigue -joint pains; muscle pains -low blood pressure At the end of naturopathic school, I was definitely into Stage 3. Luckily, there are things we can do to help you deal with the stress and rebuild the health of your adrenal glands. Do you need to put your glass down? Do you think you might suffer from adrenal fatigue? In my next blog, I will discuss testing methods for assessing the health of your adrenal glands, so that you can know which stage you’re in and we can treat more specifically based on your needs. But if you’ve read this and think you’re in the later stages based on your symptoms, don’t wait! Come on in for a visit, and I’d be happy to help you start to feel better. And don’t forget to put your glass down! References Image from 123RF.com, Copyright: https://www.123rf.com/profile_bialasiewicz'>bialasiewicz / 123RF Stock Photo</a> Selye, H. (1998). A Syndrome Produced By Diverse Nocuous Agents. Journal of Neuropsychiatry, Spring 1998; 10(2): 230-231. Scott, TD, Speidel, K. (2017). Essential Elements of Prescription Hormone Compounding. LP3 Network. Conference 2017 Apr 29-30. The connection between liver health and the skin is well-known, especially in serious liver diseases. For example, a yellowing of the skin is seen with liver cirrhosis, a condition in which scarring replaces normal functioning liver tissue. Pruritis, or skin itching, can also be associated with liver disease. The reason? The liver is one of the major detoxification organs in the body. It filters the blood and processes, breaks down, and packages major toxins (metabolites, alcohol, caffeine, medications, hormones, environmental pollutants) that your body is exposed to, in order to either make them more usable by the body, or to eliminate them. If this “processing plant” is overburdened and starts to work more sluggishly, the toxins need to go somewhere. Often, in an attempt of the body to get rid of them, many will end up in the skin, a secondary organ of elimination, and also our largest detoxification organ. Even if you don’t have a serious liver disease, your liver enzymes may not be working as optimally as they could, with repercussions showing up elsewhere, such as your skin. Therefore, in order to have healthy-looking skin, you want to make sure that your primary organs of detoxification are working properly. Supporting Your Primary Organs of Detoxification
Our primary organs of detoxification include the liver, the intestines, and the kidneys. 1) Drink Enough Water You can support kidney detoxification by drinking a sufficient amount of water, typically about 2L a day for the average person (preferably mostly away from meals to prevent diluting your digestive enzymes too much). As a rule of thumb, you should be drinking about half your body weight (in lbs) in ounces (i.e. for a 150 pound person, 150/2 = 75 oz, or roughly 9 cups). This helps you eliminate water-soluble toxins from your body, with the added bonus of plumping up your skin and decreasing the visibility of wrinkles. 2) Clean Up Your Diet Reduce foods in your diet that will put more burden on your digestive system and on your liver. This includes processed food and sugar, alcohol, caffeine, and food sensitivities. If you’re not sure about your food sensitivities, book an appointment and I’ll run a simple lab test or help you identify them through an elimination diet. You’ll also want to include foods that help improve liver function, including leafy green vegetables, cruciferous vegetables, berries, turmeric, and sufficient protein. 3) Take Probiotics Probiotics are essential for a healthy gut and immune system. They can be obtained from fermented foods in the diet, but this can be problematic since many people with skin conditions cannot tolerate cow’s dairy, including regular yoghurt. An alternative yoghurt, such as sheep or goat yoghurt, could be an option if they are better tolerated. However, probiotic supplements may be your best option. With supplements, we can be specific about which strains of probiotics we are using, as each strain has a slightly different effect on the immune system. For example, I use a different blend with a patient with acne versus someone suffering from an autoimmune condition such as psoriasis. 4) Drink Lemon Water One simple addition you can try at home that gently supports liver function is starting the day with a large glass of lemon water (about 500mL of water with the juice of about ¼ of a lemon). You’ll want to wait about half an hour before having your breakfast afterwards. Again, you don’t want to dilute your digestive enzymes! 5) Use Nutraceuticals To Support Liver Detoxification With many skin conditions, including acne and eczema, I see the fastest improvement when we include some liver supporting herbs and nutrients into the treatment plan. These can include high quality, concentrated extracts of milk thistle, dandelion, turmeric, B vitamins, and other nutraceuticals. Because these supplements can interfere with medications you are taking, or could have side-effects, work with a naturopathic doctor who can recommend the best avenue for you, monitor your progress, and modify your treatment plan if necessary. A word of caution: liver supporting herbs can initially worsen a skin condition, especially if the intestines are not working well, or if you start too much, too quickly. Do you want healthy, glowing skin from the inside out? Then making sure that your body’s primary organs of detoxification are working to your full advantage is extremely important. I can help you identify your food sensitivities, heal your digestive system, and support proper liver detoxification through an individualized program tailored to your specific needs. |
AuthorDr. Tamar Ferreira is a Naturopathic Doctor in Brampton, Ontario. Her areas of focus include digestive health, hormone balance, and skin conditions. Topics
All
Archives
May 2020
|
118 Queen St. W., Suite 205
Brampton, ON
L6X 1A5
905-451-3963











 RSS Feed
RSS Feed